
 Premier Gastroenterology Care in Sonipat
Premier Gastroenterology Care in Sonipat
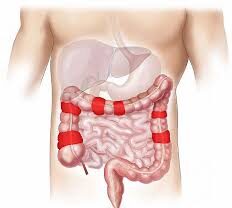
At Primax Hospital Sonipat, our Gastroenterology Department stands as the cornerstone of specialized digestive care in North India. We understand that digestive disease directly impacts your quality of life, which is why our dedicated team of expert gastroenterologists in Sonipat is committed to providing compassionate, comprehensive care for every patient who walks through our doors.
Our state-of-the-art facility combines advanced medical technology with a patient-first approach, ensuring that you receive not just treatment, but complete care tailored to your unique needs. From routine gastroenterology and digestive concerns to complex liver diseases, we’re here to restore your health and peace of mind.
Why Choose Primax Hospital for Gastroenterology Care?
🏥 Comprehensive Digestive Healthcare
- 24×7 Emergency Gastroenterology Services: Because digestive emergencies don't wait
- Advanced Endoscopy: Suites with latest technology for precise diagnosis
- Multidisciplinary Care Team including gastroenterologists, hepatologists, nutritionists, and surgeons
- Personalized Treatment Plans designed specifically for your condition and lifestyle
👨⚕️ Expert Medical Team in Gastroenterology
Our board-certified gastroenterologists in Haryana bring years of experience in:
- Complex liver disease management
- Advanced endoscopic procedures
- Inflammatory bowel disease treatment
- Minimally invasive surgical techniques
 Advanced Diagnostic Capabilities for Digestive Disease
Advanced Diagnostic Capabilities for Digestive Disease
- High-definition Endoscopy and Colonoscopy
- FibroScan for non-invasive liver assessment
- pH Monitoring for acid reflux (vomits) evaluation
- Capsule Endoscopy for small bowel examination
- Advanced Imaging (CT/MRI Enterography)
Conditions We Treat with Excellence in Gastroenterology Department
- Fatty Liver Disease
- Heartburn
- Constipation
- Ulcerative Colitis
Fatty Liver Disease – Complete Digestive Care & Management
Fatty Liver Disease is increasingly common in our modern lifestyle, but with proper care, it’s completely manageable. At Primax Hospital Sonipat, we provide comprehensive fatty liver treatment that focuses on your long-term health.
Fatty Liver Disease: Causes, Symptoms, and Treatment
What is Fatty Liver Disease? Fatty liver occurs when excess fat accumulates in liver cells, potentially leading to inflammation and liver damage. We see this condition frequently, and we want you to know – you’re not alone, and effective treatment is available.
Types of Fatty Liver: We Treat:
🔸 Non-Alcoholic Fatty Liver Disease (NAFLD)
- Simple Fatty Liver – Fat accumulation without inflammation
- Non-Alcoholic Steatohepatitis (NASH) – Fat with inflammation requiring immediate attention
🔸 Alcoholic Fatty Liver Disease (AFLD)
- Caused by excessive alcohol consumption
- Completely reversible with proper treatment and lifestyle changes
Recognizing the Signs: When to See Our Specialists
Many patients come to us asking, “How do I know if I have fatty liver?” Here are the symptoms we commonly see:
Early Stage Symptoms:
- Fatigue and general weakness
- Mild discomfort in upper right abdomen
- Often discovered during routine health checkups
Advanced Stage Symptoms:
- Unexplained weight loss
- Jaundice (yellowing of skin/eyes)
- Swelling in legs or abdomen
Our Comprehensive Fatty Liver Treatment Approach
A. Advanced Diagnostic Services:
- Liver Function Tests (LFTs) – Comprehensive enzyme analysis
- FibroScan Technology – Non-invasive assessment of liver fat and fibrosis
- Detailed Blood Work – Lipid profile, HbA1c, insulin resistance markers
- Imaging Studies – Ultrasound and advanced MRI when needed
B. Medical Management:
- Diabetes control with medications like metformin
- Cholesterol management with statins when appropriate
- Antioxidant therapy including Vitamin E and omega-3 supplements
- Regular monitoring to track improvement
C. Lifestyle Modification Program:
- Structured Weight Loss Plans: Even 5-10% weight reduction makes a significant difference
- Nutritionist Consultations: Personalized diet plans focusing on liver-healthy foods
- Exercise Therapy: Supervised fitness programs designed for your condition
- Stress Management: Because we understand the connection between stress and health.
D. Regular Monitoring & Follow-up
Since fatty liver disease can be progressive, regular check-ups with a gastroenterologist are crucial to manage and reverse the condition.
Advanced Liver Imaging (FibroScan): For accurate, non-invasive staging of fat and fibrosis.
Personalized Counseling: Diet and lifestyle guidance to prevent disease progression.
Multidisciplinary Care: Coordinated efforts from hepatologists, nutritionists, and fitness experts.
🌟 Why Choose Primax Gastro Institute?
At Primax Gastro Institute, we provide specialized and comprehensive care for fatty liver disease, focusing on:
Early Detection
Prevention
Advanced Treatment Options
Our team of expert gastroenterologists and liver specialists ensures that every patient receives personalized, evidence-based care tailored to their unique condition.
Take the Next Step
If you or a loved one is concerned about fatty liver disease, schedule a consultation with us today at Primax Gastro Institute & Super Speciality Hospital [9666460009] to take the first step toward a healthier liver and a better life.
Heartburn & Acid Reflux- Advanced Treatment Solutions in Gastroenterology Department
Heartburn might seem common, but when it affects your daily life, it needs expert attention. Our acid reflux specialists in Sonipat are here to provide lasting relief.
Heartburn: Causes, Symptoms, and Treatment
What Causes Heartburn? Heartburn occurs when stomach acid flows back into your esophagus, causing that burning sensation you know all too well. We understand how this can impact your sleep, eating habits, and overall quality of life.
Common Symptoms You can Identify:
- Spicy, fatty, or fried foods
- Coffee, chocolate, and carbonated drinks
- Large meals or eating late at night
- Stress and anxiety
- Certain medications
- Pregnancy-related changes
When to Seek Our Expert Care
Immediate Attention Needed If You Experience:
- Heartburn more than twice a week
- Difficulty swallowing
- Chronic cough or hoarseness
- Chest pain that concerns you
- Unexplained weight loss
Our Advanced Treatment Approach in Gastroenterology Department
🔍 Precise Diagnosis:
- Upper GI Endoscopy – Direct visualization of your esophagus and stomach
- 24-hour pH Monitoring – Accurate measurement of acid reflux episodes
- Esophageal Manometry – Assessment of esophageal muscle function
💊 Immediate Relief Medications:
- Antacids for quick symptom relief
- H2-receptor blockers to reduce acid production
- Proton Pump Inhibitors (PPIs) for comprehensive acid control
- Prokinetic agents to improve stomach emptying
🔬Advanced Procedures for Severe Cases:
- Fundoplication Surgery – Minimally invasive procedure to strengthen the lower esophageal sphincter
- Endoscopic Treatments – Including ARMS and TIF procedures
- GERD Surgery when conservative treatment isn’t sufficient
Why Choose Primax Gastro institutefor Heartburn Treatment?
At Primax Gastro Institute, we provide a comprehensive and personalized approach to treating heartburn and acid reflux (Gastroesophageal Reflux Disease – GERD).
Expert Gastroenterologists: Our specialists are leaders in digestive health.
Cutting-Edge Diagnostics: We use advanced techniques to accurately identify your reflux’s root cause.
Minimally Invasive Treatments: We focus on procedures and therapies that ensure lasting relief and prevent complications.
📞 Take the Next Step to Achieve Long-Term Relief
If you experience frequent or severe heartburn, don’t wait for complications.
Consult our specialists at Primax Gastro Institute & Super Speciality Hospital [9666460009] or contact us to take the first step toward long-term relief and optimal digestive health.
Constipation: Comprehensive Management & Relief
Chronic constipation can significantly impact your quality of life. Our constipation specialists understand your discomfort and provide effective, long-lasting solutions.
Understanding Constipation: We define constipation as:
- Fewer than three bowel movements per week
- Hard, dry, or lumpy stools
- Straining or difficulty passing stools
- Feeling of incomplete evacuation
Root Causes We Address:
Lifestyle Factors:
- Low fiber intake
- Inadequate hydration
- Sedentary lifestyle
- Ignoring natural urges
Medical Conditions:
- Irritable Bowel Syndrome (IBS-C)
- Thyroid disorders
- Diabetes complications
- Neurological conditions
Medication-Related:
- Opioid painkillers
- Iron supplements
- Certain antidepressants
- Blood pressure medications
Our Treatment Approach
🔬 Advanced Diagnostics:
- Colonoscopy – To rule out structural problems
- Anorectal Manometry – Evaluates muscle function
- Transit Studies – Measures digestive system speed
💊 Comprehensive Treatment:
First-Line Treatments:
- Bulk-forming laxatives (psyllium, methylcellulose)
- Osmotic laxatives (polyethylene glycol, lactulose)
- Stool softeners for easier passage
Advanced Therapies:
- Biofeedback Therapy – Retraining pelvic muscles
- Sacral Nerve Stimulation – For severe cases
- Nutritional Counseling – Personalized fiber and fluid recommendations
🚽 Why Choose Primax Gastro Institute for Constipation Treatment?
Multidisciplinary & Evidence-Based Care: At Primax Gastro Institute, we provide comprehensive, evidence-based treatments for chronic constipation, ensuring personalized care tailored to each patient’s condition.
Expert Team Approach: Coordinated care from:
Expert Gastroenterologists
Dietitians
Physiotherapists
Goal: To provide effective long-term relief and improved digestive function.
📞 Take the Next Step
Start Your Path to Relief: If you’re struggling with persistent constipation, it’s time to seek specialized help.
Contact Primax Gastro Institute & Super Speciality Hospital [9666460009] to schedule a consultation and take the first step toward better digestive health.
Ulcerative Colitis Expert IBD Management
Ulcerative Colitis (UC) is a serious condition that requires specialized care. Our IBD specialists in Haryana provide comprehensive management to help you achieve and maintain remission.
What is Ulcerative Colitis?
UC is a chronic inflammatory bowel disease affecting the colon and rectum. We understand this is a life-changing diagnosis, but with proper treatment, most patients live full, active lives.
Symptoms We Help Manage:
- Frequent, bloody diarrhea
- Abdominal pain and cramping
- Urgency and incomplete evacuation
- Fatigue and weakness
- Unintended weight loss
- Joint pain and skin problems
Our Comprehensive UC Treatment Program
🔬 Precise Diagnosis:
- Colonoscopy with Biopsy – Gold standard for UC diagnosis
- Advanced Blood Tests – Inflammation markers and nutritional status
- Stool Analysis – Including fecal calprotectin
- Imaging Studies – CT/MRI when needed
💊 Advanced Medical Therapy:
First-Line Treatments:
- 5-ASA medications (Mesalamine, Sulfasalazine)
- Corticosteroids for acute flare-ups
- Immunomodulators (Azathioprine, Methotrexate)
Advanced Biologics:
- Anti-TNF therapy (Infliximab, Adalimumab)
- Anti-integrin therapy (Vedolizumab)
- JAK inhibitors (Tofacitinib)
🏥 Surgical Excellence: When surgery is needed, our expert surgeons perform:
- Proctocolectomy with IPAA – Advanced reconstructive surgery
- Minimally Invasive Techniques – Faster recovery, better outcomes
Ulcerative Colitis (UC) Treatment Approach
At Primax Gastro Institute, our expert gastroenterologists and IBD specialists provide personalized treatment plans for Ulcerative Colitis, including:
State-of-the-Art Endoscopic Diagnostics: Accurate assessment and monitoring of disease activity.
Advanced Medical Therapies: Access to the latest treatments like biologics and JAK inhibitors.
Advanced Surgical Treatment: Expertise in procedures like Proctocolectomy with Ileal Pouch-Anal Anastomosis (IPAA) when necessary.
📞 Schedule a Consultation
Take the Next Step Toward Relief: If you are experiencing persistent digestive issues or UC symptoms, don’t delay expert care.
Schedule a consultation at Primax Gastro Institute & Super Speciality Hospital [9666460009] for expert care and long-term relief.
Why Primax Gastro Institute is the Best for Gastroenterology in Sonipat?
Advanced Endoscopy and Minimally Invasive Surgeries
Experienced and Certified GI Specialists
Integrated Care: From Precision Diagnosis to Follow-ups
Advanced Emergency Care with State-of-the-art ICU Support
Patient-First Philosophy: Comfort, Dignity & Transparency
24/7 Emergency Support with Lifesaving Care

Our board-certified gastroenterologists and hepatologists provide comprehensive, specialized care for the full spectrum of digestive, intestinal, and liver disorders. This includes:
Common Gastrointestinal (GI) Issues: Chronic Acid Reflux (GERD), Peptic Ulcers, Gastritis, Dyspepsia, and Functional GI disorders.
Inflammatory Bowel Disease (IBD): Advanced management of Crohn’s Disease and Ulcerative Colitis.
Liver Disease: Expert diagnosis and treatment for conditions like Hepatitis, Fatty Liver Disease (NAFLD/NASH), Cirrhosis, and Liver Cancer.
Pancreatic & Biliary Disorders: Pancreatitis, Gallbladder stones, and other complex bile duct conditions.
Colorectal Health: Screening, surveillance, and removal of Colorectal Polyps, as well as treatment for Colorectal Cancers.
Nutritional & Absorption: Management of Celiac Disease, Irritable Bowel Syndrome (IBS), Malabsorption Syndromes, and Chronic Diarrhea
Primax Gastro Institute utilizes state-of-the-art endoscopic technology to ensure highly accurate diagnosis and minimally invasive treatment. Our advanced procedures include:
Diagnostic & Therapeutic Endoscopy: Standard Upper Endoscopy (EGD) and Colonoscopy with high-definition imaging for early detection of polyps and lesions.
Endoscopic Ultrasound (EUS): Used for advanced staging of cancers and detailed imaging of the pancreas, bile ducts, and GI wall.
Endoscopic Retrograde Cholangiopancreatography (ERCP): A specialized procedure for treating stones, strictures, and tumors in the bile ducts and pancreas.
FibroScan Technology: Non-invasive liver elastography for assessing liver fat and fibrosis (scarring).
Scheduling a consultation is quick and easy. We offer multiple convenient options:
By Phone: Call our dedicated appointment line at [9666460009] to speak directly with our scheduling coordinator.
Online Booking: Visit the ‘Book Appointment’ or ChatNow button at the bottom of the section on our site.
In-Person: You may visit the registration desk at Primax Gastro Institute & Super Speciality Hospital during business hours.
We encourage new patients to bring any relevant past medical records or test results to their initial visit.
Your initial consultation with our GI specialist is an important steps in establishing an accurate diagnosis and personalized care plan. You can expect:
Detailed Medical History: The specialist will thoroughly review your symptoms, dietary habits, family history, and any previous tests or treatments.
Physical Examination: A focused physical exam will be performed.
Next Steps Discussion: The physician will explain the potential causes of your symptoms and outline a diagnostic strategy, which may include blood tests, stool analysis, or an endoscopic procedure (like a colonoscopy or EGD).
Personalized Treatment Plan: We will discuss preliminary lifestyle and nutritional recommendations and ensure all your questions are answered, empowering you to take charge of your digestive health.
Absolutely. We recognize that IBD (Crohn’s Disease and Ulcerative Colitis) requires lifelong, collaborative care. Our institute specializes in multidisciplinary IBD management, which includes:
Customized Treatment Plans: Utilizing advanced medical therapies, including biologics and Janus kinase (JAK) inhibitors, to achieve and maintain remission.
Nutritional Guidance: Consulting with specialized dietitians to manage dietary triggers and prevent deficiencies.
Surgical Evaluation: Seamless coordination with our advanced surgical team for patients requiring intervention.
Continuous Monitoring: Regular follow-up and advanced diagnostic checks to prevent flare-ups and screen for complications.



